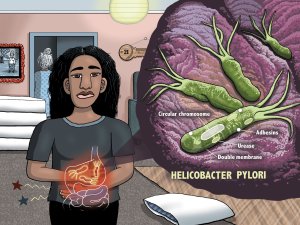
Academic pharmacist Nataly Martini provides key information on Helicobacter pylori pathophysiology, diagnosis and evidence-based treatment strategies to enhance patient outcomes
Te Whatu Ora breaches Code in care of man with severe lung condition - 21HDC00863
Te Whatu Ora breaches Code in care of man with severe lung condition - 21HDC00863
The Deputy Health and Disability Commissioner has found Waitematā District Health Board DHB (now Te Whatu Ora Waitematā) breached the Code of Health and Disability Services Consumers' Rights (the Code) in its care of a man with a severe and progressive lung condition. Sadly, the man, in his sixties, passed away as a result of the condition.
Deborah James found Te Whatu Ora breached Right 4 (1) of the Code - the right to services of an appropriate standard provided with reasonable care and skill.
The breach concerns the assessments, communication and support referrals made for the man who wished to receive palliative treatment at home by two hospitals of the Waitematā DHB in 2020.
Ms James was critical of the way the man’s discharge and palliative care was managed.
"Mr B was not reviewed by an occupational therapist or physiotherapist prior to discharge …. A physiotherapy and occupational therapy assessment, including a home visit prior to discharge, would have allowed for the necessary equipment to be in place to allow [Mr B] to be as comfortable as possible in his last days of life," she said.
Ms James noted the man’s partner of many years was unclear about the oxygen delivery plan and about the oxygen saturation settings for the palliative oxygen care at home. She said overall communication with the man and his partner was poor, leaving his partner feeling confused about the progress of the man’s condition while he was in hospital, and about the timeframe for appropriate hospice support after discharge.
Ms James’ report notes that the man would have benefitted from hospital palliative care involvement and, under the man’s circumstances, inpatient palliative care assessment should have been standard care. She noted that if all the appropriate assessments prior to discharge had been done, the man and his partner would have received more support at home.
Te Whatu Ora has advised HDC that since the complaint it has ensured medical wards have access to inpatient palliative care services to refer patients to, if needed. It has made sure there are multi-disciplinary team meetings on the ward and that family can meet with these teams. It also now recommends GPs are notified directly of their patient’s discharge - particularly on a Friday or over the weekend. Finally, it has developed and put in place the Hospital in the Home (HiTH) service which provides clinical monitoring phone or telehealth monitoring for discharged patients for the Waitematā region.
Ms James acknowledged these changes and has requested Te Whatu Ora update her with its discharge policy within six months of this report. She has also requested:
- The materials and attendance list for training and education on using oxygen cylinders at home.
- A review of policy/guidance for hospice referrals to ensure a call is made by medical team member on the day of a patient’s discharge if they need urgent or palliative care.
- Confirmation of training of staff on making clear notes and documentation.
- That Te Whatu Ora review the process of transferring patients between hospitals.
Ms James has asked Te Whatu Ora to report on any changes made as a result of her review and provide evidence of those changes; and requested Te Whatu Ora review the effectiveness of HiTH and consider using it across other districts if found to be successful.
Ms James also made an adverse comment about the communication and documentation by a doctor involved in the man’s care. She has asked the doctor and Te Whatu Ora to provide a written apology to the deceased man’s partner.