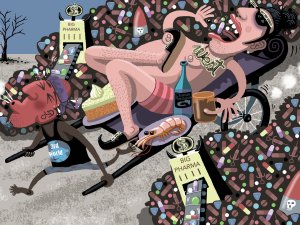
In this article, Sue Frankland looks at the global problem of wastage of medications, including causes such as overprescribing and non-adherence. She also presents information from her master’s dissertation on how people understand, and respond to, medication expiration dates
Response to report into Waitakere Hospital staff infected with COVID-19
Response to report into Waitakere Hospital staff infected with COVID-19

13 May, 2020
Waitematā District Health Board (DHB) is deeply sorry that staff who were caring for patients from St Margaret’s Hospital and Rest Home have tested positive for Covid-19.
Deputy CEO Dr Andrew Brant said a report released today into the circumstances of the first three nurses on the ward who returned positive tests would be used to improve how similar situations were managed in future.
“We are deeply saddened that these nurses became infected with Covid. They were being selfless in caring for others in the middle of a difficult, evolving and intense situation at St Margaret’s.
“We recognise their professionalism in caring for patients from St Margaret’s and we regret that they became ill in the course of their work.”
Dr Brant said the report – with independent panel members including the Chief Nurse and Midwifery Officer at Waikato DHB and a NZ Nurses’ Organisation representative - set out the chain of events which led to three nurses initially becoming infected.
A further four nurses who also worked on the Covid ward at Waitakere Hospital have subsequently tested positive.
Waitakere Hospital agreed to accept the transfer of six Covid-positive residents from St Margaret’s Hospital and Rest Home in Te Atatu on 17 April due to significant concerns for the viability of the facility as part of an emergency response to a rapidly evolving situation.
Dr Brant said Waitematā DHB contributed its own staff to run St Margaret’s at the same time as accepting Covid-positive residents as inpatients amid the uncertainty of the evolving COVID-19 pandemic.
“This required rapid action and decision-making in the middle of the highly pressured, evolving situation.
“Although we prepared as best we could, admitting Covid-positive St Margaret’s residents has caused stress to our DHB and our staff.
“The report released today shows our staff were well-trained and personal protective equipment (PPE) was used at all times. We have also had confirmation that preparations at Waitakere Hospital were well-advanced to receive and look after Covid patients. “However, there are clearly some things we could have done better and which we need to learn from.”
This included:
• Better-communicating decisions between clinical staff to help them understand the basis for those decisions, particularly where they needed to be made rapidly in response to an emergency situation.
• Having better systems in place to capture and respond quickly to staff concerns and feedback.
• Finding a way of ensuring better consistency of the national PPE supply, reducing the need to change products in the middle of responding to a pandemic, which caused significant concerns to staff.
• Developing a national plan on how DHBs should appropriately support aged care facilities when the health system is already responding to a crisis.
“There are some key things we can learn from this review and we are happy to share what we’ve found with other DHBs across the country,” Dr Brant said.
“We are committed to driving improvement and working with our staff and unions to ensure that what has happened at Waitakere Hospital serves as a catalyst for positive change.”