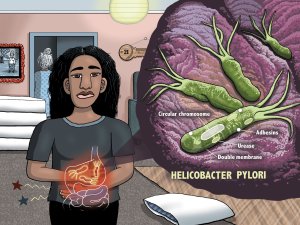
Academic pharmacist Nataly Martini provides key information on Helicobacter pylori pathophysiology, diagnosis and evidence-based treatment strategies to enhance patient outcomes
Budget 2023: Government tackles winter, waitlists and workforce
Budget 2023: Government tackles winter, waitlists and workforce

- More than $1 billion allocated to increase health workforce pay rates and boost staff numbers
- Investment to allow for 500 new nurses
- Major investment to reduce waiting lists
- $20 million to lift immunisation and screening coverage for Māori and Pacific peoples
The Chris Hipkins Government is tackling pay and workforce pressures in the health system with a billion dollar boost that will increase pay rates and the number of nurses.
“The Budget is focused on three service priorities – winter, workforce and waitlists, as we build a more equitable health system,” Ayesha Verrall said.
Budget 2023 marks the second year of multi-year funding, with a $1.3 billion increase to address health cost pressures.
Workforce
“To help stabilise our workforce, we are investing over $1 billion in increasing health workers’ wages and boosting staff numbers, with a focus on areas facing greatest demand,” Ayesha Verrall said.
The funding includes $63 million for progressing safe staffing and allows for an additional 500 new nurses to be employed.
“Budget 2022 invested $76 million over four years to develop the health workforce, with a focus on primary care and nurses.
“Key targeted workforce initiatives such as Te Pitomata grants for tauira Māori and Ngā Manukura o Āpōpō nursing and midwifery leadership training will remove barriers to more responsive training pathways, increasing recruitment, and improving immigration processes to alleviate workforce shortages,” Ayesha Verrall said.
The health reforms enable long overdue action on workforce training and region. Further initiatives, including priority actions identified by the workforce taskforce, will be enabled by Budget 2023 funding.
Prioritised spending for 2023/2024
“Around $99 million is being put towards the coming winter, focused on providing primary and community care closer to people’s homes, reducing pressure on hospitals, and speeding up discharge from hospitals through community-based care for older people.
“$118 million has been allocated to help reduce waiting lists by improving patient flow, enabling planned care to be delivered in primary settings and freeing up inpatient hospital beds, allowing for surgeries to go ahead.
“We are spending $20 million to establish outreach services to lift immunisation and screening coverage for Māori and Pacific peoples, and implement approaches and improvements in care and treatment that increase life expectancy of Māori and Pacific peoples,” Ayesha Verrall said.
Primary and community care
“Primary and community care are key to reducing pressure on hospital services and providing people the care they need when and where they need it,” Ayesha Verrall said.
“In 2023/24, we are putting an extra half a billion dollars into primary and community care sector, to support sector stability and to reduce pay disparities overtime between hospital and community health sector staff.
“I recently announced funding of $44 million over two-years for primary care providers serving communities with the highest needs in New Zealand. This funding will support the establishment of comprehensive primary care teams, build capacity in the workforce, and address the burden of under-funding for Māori and Pacific providers. We will also allocate $4.9 million for the training and development of the new kaiāwhina workforce to support these teams.
“A targeted investment of $37 million over the next two years will more equitably allocate primary care funding to general practices based on their enrolled high-needs populations, and those providers with the highest Māori and Pacific populations.
“As part of this boost to strengthen primary, community and rural care, to support the winter pressures, we’re funding up to 193 additional frontline clinical team members across the country to focus on early intervention, faster treatment and better support for whanau.
“We are also well aware of how important both physical and mental health is for our rangatahi and through historic investment have expanded our School Based Health Services to over 300 decile 1-5 secondary schools. Around 96,000 students have access to nurses who can support mental wellbeing at school,” Ayesha Verrall said.
A sustainable budget for the future
In the first month of the reforms savings were made in insurance costs which were used for workforce initiatives, including funding more primary care, GP training placements, subsidies for return to work and internationally qualified nurses to work in New Zealand, and additional training placements for nurse practitioners.
Since the health reforms, there has been savings of more than $10 million with the dis-establishment of executive leadership roles of the former District Health Boards.
“From 2024, it is our intention that future health budgets will move to a three-year funding cycle to align with the first three-year New Zealand Health Plan, due in 2024,” Ayesha Verrall said.