Academic pharmacist Nataly Martini provides key information on Helicobacter pylori pathophysiology, diagnosis and evidence-based treatment strategies to enhance patient outcomes
Webinar: Intensifying insulin therapy for people with type 2 diabetes
Webinar: Intensifying insulin therapy for people with type 2 diabetes
This webinar provides an update on when and how to intensify insulin therapy for patients with type 2 diabetes. It is the fourth in a series of webinars on the management of diabetes, brought to you with the support of Sanofi
This activity has been endorsed by the Pharmaceutical Society of New Zealand as suitable for inclusion in a pharmacist’s continuing education records for continuing professional development purposes. You can record details of this webinar on the “Keeping up to date” page of your portfolio on MyRecert (myrecert.pharmacycouncil.org.nz).
This webinar is presented by endocrinologist Rosemary Hall and has the following learning objectives:
- Describe factors for consideration when initiating and intensifying insulin in patients with type 2 diabetes, including insulin type, dose, timing and titration.
- Identify practical aspects of patient care associated with taking insulin.
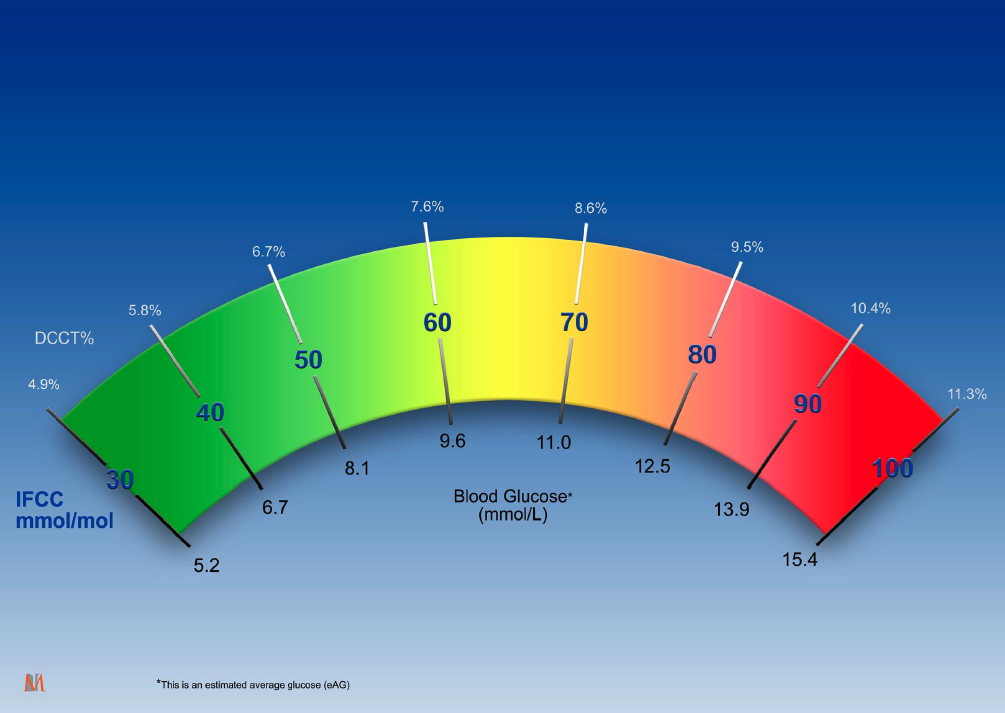
- Discuss potential outcomes associated with increasing HbA1c levels, and the place of target HbA1c levels.
- List primary aims of the New Zealand Society for the Study of Diabetes Type 2 Diabetes Management Guidance and identify treatment options for glycaemic control.
After you have watched this presentation, you may complete the assessment below to test your understanding of the topic.
Remember, you can also use the Capture button below to record your time spent watching.
This is the fourth webinar in a series on the management of diabetes.
Watch the first webinar in this series: Update on interventions to improve glycaemic control in type 2 diabetes
Watch the second webinar in this series: Insulin therapy for patients with type 2 diabetes
Watch the third webinar in this series: Practical management for patients with diabetes
This 10-question multiple-choice assessment is designed to demonstrate that the webinar has been effective in allowing you to meet the learning objectives of this course. Write down your answers to these questions.
1. What is an appropriate starting dose for most people when initiating basal insulin?
a. 10 units per day
b. 20 units per day
c. 40 units per day
d. 60 units per day
e. 1 unit per kg
2. When is an appropriate time to administer insulin in people initiating this therapy?
a. At lunchtime if glucose levels tend to rise throughout the day
b. At night time if glucose levels are the highest then
c. Every second day in the morning
d. The time of day the patient will find the easiest to take the insulin regularly
3. A critical feature of premix insulins is that:
a. dose reduction is not needed when meal size is significantly reduced from normal
b. peak insulin levels are achieved 15 minutes after each dose; effect time is four hours
c. there is no need to mix the insulin pen contents before administration
d. they must be given at a meal time
4. Once you are taking bolus insulin, you have to take it at every meal. True or false?
a. True
b. False
5. Patients with diabetes can expect that once on insulin, they will have:
a. a somewhat decreased quality of life, with lower energy levels
b. far fewer hypoglycaemic episodes
c. freedom to eat more freely and flexibly
d. to accept a lifelong commitment to insulin therapy
e. weight loss
6. How do you determine the time of day for adding prandial insulin to achieve the most benefit?
a. Assess each day’s meals, and choose the best time each day based on the meal’s protein content
b. Choose the meal time when blood glucose levels are the highest afterwards
c. Dinner time is always best as that is the time of most insulin resistance
d. Select the meal time in which the meal is likely to be digested the fastest
7. For what TWO reasons may it be more appropriate to set an HbA1c target of >53mmol/L?
a. When the patient has a shorter life expectancy
b. When the patient has had previous significant unawareness of hypoglycaemic episodes
c. When the patient is able to self-fund the newer diabetes medicines
d. When the patient is an adolescent
e. When the patient is newly diagnosed with diabetes
8. What are potential clinical outcomes if HbA1c levels increase over time?
a. Amputations from peripheral vascular disorder
b. Microalbuminuria
c. Myocardial infarction
d. Nephropathy
e. Neuropathy
f. Retinopathy
g. All of the above
9. One of the main aims of the NZSSD Type 2 Diabetes Management Guidance is to:
a. delay insulin therapy for as long as possible
b. move practitioners away from standard older therapies to the newer medicines
c. reduce clinical inertia and recognise when a patient’s diabetes management needs to be reviewed
d. shift from a risk-based to a glycaemic-based diabetes management approach
10. In patients with diabetes and predominately heart failure or diabetic renal disease, which initial second-line agent would generally be preferrable?
a. Dipeptidyl peptidase-4 inhibitor
b. Glucagon-like peptide-1 receptor agonist
c. Sodium-glucose cotransporter-2 inhibitor
d. Thiazolidinedione
Write down your answers to these questions. Then, to check your answers and record your score, click here.