Academic pharmacist Nataly Martini discusses the medical management of asthma in adults and adolescents, which has evolved to prioritise early anti-inflammatory treatment. She also explains how to improve patient outcomes by proactively identifying poor asthma control and supporting equitable access to education and treatment
Waging war on influenza and the common cold
Waging war on influenza and the common cold
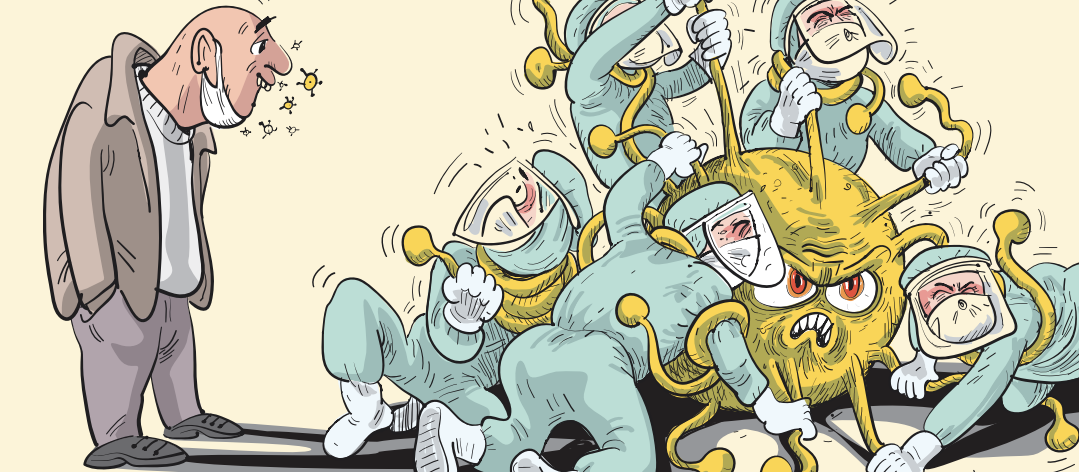
Non-practising pharmacist Sarah Mooney looks at the differences between influenza and the common cold, then discusses defensive and offensive strategies to combat these viral diseases
Many people do not understand the severity of influenza and often mistake it for a common cold
In the olden days, French scientist Louis Pasteur discovered the process of pasteurisation by testing the hypothesis that microbes enter liquids through particles of dust in the air. His findings laid the foundation for the germ theory of disease, which ultimately enabled the development of strategies to prevent and treat diseases, including vaccines that helped eradicate smallpox.
Despite the progress, millions still die each year from influenza, with poor uptake of flu vaccines and hygiene practices, and quickly evolving viruses contributing to the problem. A misinformed public worsens the situation as many people do not understand the severity of influenza and often mistake it for a common cold – how many times during the COVID-19 pandemic did we hear a vocal minority say “COVID is no worse than the flu”!
Pharmacies can play an essential role in educating patients about the difference between the two and encouraging them to get vaccinated. Strategies such as containment, prevention and having empathetic conversations with anti-vaxxers can help combat the problem. Pharmacy staff can offer face masks, hand sanitiser and disposable tissues to sick patients to stop the spread of the virus, in addition to education.
Pharmacies can also now provide funded influenza vaccinations at the same time as the COVID-19 vaccine booster. To confront anti-vaxxers, empathetic listening can be more effective than direct confrontation. By reflecting on a patient’s desire to protect their loved ones, pharmacists can help change their behaviour.
Every year, scientists around the world use a statistical crystal ball to try to predict which strains of influenza will be the most prevalent that season, in an effort to mount a defence. However, even with vaccination and modern medical science, 150 years since the discovery that microbes cause disease, millions still die each year from the deadly virus. Poor uptake of the influenza vaccine and a quickly evolving virus means front-line health professionals still have a long battle ahead against the disease.
Everyone has encountered someone sneezing and sniffing while out and about who makes an offhand comment about “having a bout of flu”. Public sentiment is still apathetic about the seriousness of influenza, despite extensive public health campaigns on the subject. A misinformed public that does not understand the seriousness of influenza worsens the apathy towards getting vaccinated and isolating when sick.
Both influenza and rhinovirus are viruses that cause upper respiratory tract infections. However, influenza can kill even healthy adults and may require extensive rehabilitation and time off work, whereas rhinovirus causes the common cold, which will only lead to complications in those who are already sick or immune suppressed.
Influenza symptoms may include headaches, vomiting, fever, sore throat, fatigue and muscle aches. Symptoms of rhinovirus (common cold) may include nasal congestion, sneezing, cough, watery eyes and rarely a fever. Both share symptoms with COVID-19, so a rapid antigen test should be done when patients have any of these symptoms. Pharmacies are in an excellent position to educate patients on the differences between colds and flu and recruit them to defence.
Containment – as both influenza and the common cold are caused by airborne viruses, asking sick patients to wear masks is a cost effective and practical approach to stopping the spread of disease. Encourage staff to offer a face mask, hand sanitiser and disposable tissues every time a patient comes in to purchase an over-the-counter cold remedy, and consider placing these in the cold section if possible. Dettol spray disinfectant (and others) can be used in the air to kill airborne virus particles and could be offered if available.
Prevention – pharmacist vaccinators are able to provide funded influenza vaccinations to eligible persons over three years old, and non-funded vaccinations to anyone over 12 who is ineligible for a funded vaccine. All persons from age three receive Afluria Quad – a vaccine that protects against four strains of influenza.
Pharmacists must complete an Immunisation Advisory Centre (IMAC) training course, a practical and written assessment, acquire a CPR and anaphylaxis first aid qualification, and notify the Pharmaceutical Society of New Zealand that they are now vaccinating. There are ongoing recertification requirements for both IMAC and first aid, so it pays to set up a reminder when renewals are due.
Pharmacies providing influenza vaccinations must have sharps disposals, adrenaline kits and a second person with first aid qualifications available. They must have consent forms, patient information leaflets, standard operating procedures (SOPs) and achieve Cold Chain Accreditation.
The Pharmacy Guild of New Zealand and Green Cross Health have excellent resources available to members, including break-even calculators, SOPs, marketing materials and other documentation. Te Whatu Ora also sends out free vaccination public health campaign materials for pharmacies to use.
It is worthwhile to directly market to local businesses the availability of vaccines at the start of the season as this may reach consumers who are too busy to get to their general practice for vaccinations. The more people who are vaccinated, the more effective the vaccines will be.
Confronting anti-vaccine sentiment – despite extensive evidence of the safety of vaccines, the health profession is still faced with disheartening negative sentiment towards vaccinations, with the internet and social media providing a ready source of information to feed people’s fears. Even members of the public that would not consider themselves as “anti-vaxxers” may be against influenza vaccination because of the aforementioned complacency towards the disease – that it’s “only the flu”.
Another common misconception is that the vaccine might give them the disease – “every time I have had the flu shot in the past, I have been sick immediately afterwards”. The IMAC education team discusses this response during the vaccinator training course, telling vaccinators that while a short-term reaction to the vaccine may occur, including low fever and pain at the injection site, this reaction actually means your body is showing a very good immune response to the vaccine, and getting influenza would be far worse.
Using an empathetic response to anti-vaccination sentiment will always be more effective than confrontation and trying to argue the point. As described in the book Motivational Interviewing in Healthcare: Helping Patients Change Behavior by Stephen Rollnick and colleagues, arguing the opposite side of an argument will almost always see a patient defend the side the clinician is arguing against. A better approach is to listen for suggestions that a patient may want to change their behaviour (eg, “I want to protect my loved ones from influenza”) and reflect these statements back to them.
Inevitably, we have to treat colds and flu; the average adult gets four to five colds per year
Inevitably, we have to treat colds and flu; the average adult gets four to five colds per year. Treating each symptom individually is more efficacious than any single pill remedy; however, many patients want the convenience of one product over several, despite a pharmacy’s best efforts to educate.
Analgesia – a 2015 study by Freeman and Quigley (N Z Med J 2015;128[1424]:28–34) found that in the Wellington Regional Hospital emergency department, paracetamol was the most common cause of medication poisoning, accounting for 23 per cent of attendances for medication poisonings, which is in line with other developed nations. Yet, it is sold in pharmacies, supermarkets and petrol stations.
For this study, the authors also examined several New Zealand-operated online pharmacies and found that most were selling bulk packs of paracetamol (100 tablets of 500mg) with no checks in place as to who was completing the purchase. While this is completely legal, it does raise the issue of whether this is ethical – pharmacies have a duty of care to prevent poisoning when they sell paracetamol-containing products.
Unfortunately, for unsuspecting consumers, the variety of products that contain paracetamol is relatively large and auspicious. Anecdotally, many consumers don’t realise that the popular Lemsip product contains paracetamol and will drink the sachets as well as take a cold and flu combination remedy, or they will drink more than the maximum daily dosage.
Because paracetamol is the first drug of choice of prescribers for analgesia, and so readily available, many in the general public are unaware of how little of an overdose can cause irreversible damage. That being said, at the recommended dose, it remains the first choice of analgesia for mild to moderate pain. Pharmacy staff should try to educate consumers on the risks of paracetamol at every sale, and if an overdose has already occurred, ring the National Poisons Centre (0800 764 766) for advice, even if the patient seems fine.
Topical NSAIDs – using a local NSAID is a great way to soothe very sore throats. NSAIDs are available in sprays and lozenges. If the patient needs an economic alternative, soluble aspirin dissolved in half a glass of warm water can be gargled for a few minutes to great effect. This is also an option to offer prescribers looking for a funded prescription item for throat pain.
Decongestants – xylometazoline and saline nasal irrigation offer the best efficacy.
Rest and monitor – ensure the patient has a quality thermometer, that they know how to use it and when to seek help. A fever (>38°C) in children under three months of age requires referral to the doctor, or over 39°C in children aged three to six months. However, parents should trust their gut as many store-bought thermometers are unreliable. As patients will frequently present to the pharmacy before taking their or their child’s temperature, it may be a good idea to keep a thermometer with a reusable probe at the pharmacy. The patient’s temperature may be taken in store to help with the decision to refer and reduce delays in treatment if referral is necessary.
Unwell adults should always call Healthline first, rather than go to a pharmacy or medical centre and risk spreading the virus. Healthline have trained triage nurses to determine whether they can continue with self-care or need to present to their GP. Those who are severely immune suppressed or have been previously hospitalised by influenza should check in with their primary health provider.
For self-care, the patient will unlikely feel like eating or drinking, especially if they have influenza, so encouraging regular sipping of fluids in the form of electrolytes is prudent. Of course, honey and lemon drinks never go astray, and you can’t go past a bowl of homemade chicken soup!
Sarah Mooney is a Christchurch pharmacist on the non-practising register pursuing postgraduate studies while raising a young family





