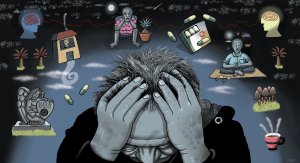
This article, written by Sidhesh Phaldessai, provides an overview of geriatric psychopharmacology, including the epidemiology of mental health disorders in the older population, the physiological changes that occur with ageing and their impact on pharmacokinetics and pharmacodynamics, and the use of psychotropic medications in older adults
Tighter gestational diabetes control good for babies
Tighter gestational diabetes control good for babies

A large study of Aotearoa New Zealand’s shift to tighter control of gestational diabetes finds improved outcomes for newborns.
Babies’ birth injuries and deaths have been reduced with the introduction of stricter diabetes controls across hospitals in Aotearoa New Zealand, new University of Auckland research finds.
Women with gestational diabetes can change their diet and take medication, if needed, to control their blood sugar levels, but it has been unclear how tightly those levels should be controlled to minimise the risks to the mother and baby.
The Liggins Institute-led researchers studied pregnant women with gestational diabetes as the new tighter targets for blood sugar were introduced following Ministry of Health recommendations in 2014.
They compared more than 500 women where the older, less tight blood sugar targets were applied and a similar number with the new tighter targets. See PLOS Medicine (8 September 2022).
“We expected to see fewer large babies and did not, but we saw benefits for babies, including a reduction in serious health problems that included deaths,” says lead researcher Professor Caroline Crowther.
However, to the researchers’ surprise, the tighter blood-sugar control increased the risk of serious health outcomes for the mother, although these events were rare.
“Individual health problems weren’t statistically significant but, as a composite they were,” Crowther says. “The largest contributor was major haemorrhage, which is not known to be linked to gestational diabetes. These findings remain unexplained.”
Further research is needed in a variety of healthcare settings, Crowther says.
The Liggins-led group plans to follow-up the mothers and babies four years’ after the birth. They will assess the metabolic health of the mothers and the size of the children, as well as incidence of obesity and diabetes, which are associated with gestational diabetes.
Liggins researchers estimate over six percent of New Zealand women or about 3,800 per year develop diabetes during pregnancy, with Māori, Pacific and Asian women over-represented.
This study follows publication of another trial, also led by Crowther, comparing diagnostic thresholds for gestational diabetes, which supported diagnosis at a lower blood sugar level than currently recommended in New Zealand. This was associated with a greater number of interventions, but better outcomes for mothers and babies when mild disease was detected and treated. See New England Journal of Medicine 18 August 2022.
Both studies responded to research questions posed by the New Zealand Ministry of Health following the guidelines review in 2014.
Liggins director Professor Frank Bloomfield says, “The Liggins Institute, which celebrates its 21st anniversary this year, is well set up to conduct these large trials that inform healthcare internationally. These trials will provide valuable information for updating the national gestational diabetes guidelines.”