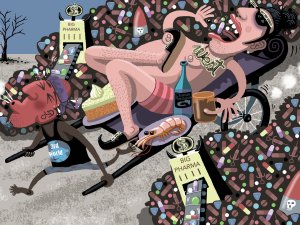
In this article, Sue Frankland looks at the global problem of wastage of medications, including causes such as overprescribing and non-adherence. She also presents information from her master’s dissertation on how people understand, and respond to, medication expiration dates
Who is Ashley Bloomfield? Delving into the New Zealand Doctor archives
Who is Ashley Bloomfield? Delving into the New Zealand Doctor archives

For the last few weeks, the daily voice of calm in the turbulence that is the COVID-19 pandemic has been director-general of health Ashley Bloomfield. He took the day off yesterday but is back on board today. From the New Zealand Doctor archives comes the following profile of Dr Bloomfield written in August 2018 not long after he stepped into health's top job
Incorrect figures appeared in the 2017 Budget documents, disputes between staff and Canterbury DHB were aired publicly, and a DHB chief executive’s personal spending of public funds went undetected. Can the Ministry of Health recover from recent lows? Virginia McMillan meets the new boss
Rumour and dismay have been rife in recent years when health professionals talked about the Ministry of Health. Recurring themes were low morale, lack of direction, faulty implementation of programmes and poor communication.
New Zealand Doctor has heard sector experts describe the ministry as a disaster zone in which capability and credibility were destroyed.
The boil was lanced in December 2017.
The State Services Commission rated as weak the ministry’s leadership and governance, values and culture, people management and staff engagement, and collaboration and partnerships. It came in the commission’s five-yearly review of performance.
Although some health organisations say they had no problems in their relationships with the ministry, many of them say the opposite.
The new holder of the seat of power works in a modest office on the first floor of the ministry’s Wellington headquarters, with no glorious harbour views. Director-general of health and ministry chief executive Ashley Bloomfield says it’s an improvement on an aged DHB building he has recently worked in.
From that “side of the fence”, he had a strong sense that people wanted the ministry to be deeply engaged and to succeed, Dr Bloomfield says.
“Because, actually, they see that a successful and effective ministry is fundamental to the wider sector being successful and effective.
“So there is enormous goodwill for the ministry to, in effect, up its game and work differently with the sector.”
On primary care: The stated intention of a more prominent role for primary care hasn’t eventuated
DR BLOOMFIELD, a 1991 medical graduate with a master of public health, has lived in Wellington for most of the past 20 years. He is married to an Auckland Medical School classmate, Libby; they have three children, one at university and two at secondary school.
He says he wasn’t confident of selection against the 26 other applicants to head the ministry. He had missed out on jobs in the past but had long thought that, “if the opportunity came up, I would see where I was at”.
That opportunity arose with the resignation last December of Chai Chuah, two years before his contract would have expired.
Dr Bloomfield, meanwhile, was about to start as acting chief executive at Capital & Coast DHB on secondment from the top job at Hutt Valley DHB. He “absolutely loved” his job.
Earlier in the year, he had undertaken additional training in strategic leadership at Oxford University. He threw his hat in the ring, the commission got enthusiastic endorsements from his referees and the job was announced as his in May.
What Dr Bloomfield is confident about is the “suite of experience” he brings to the job. It comes from being “a lifer in health”, as he puts it. (See “Bloomfield in brief”, this page.)
Speaking in his first media interview since starting in the job on 8 June, he says he has followed on from Stephen McKernan – who acted in the role for four months – in shifting the way the ministry was relating to the sector.
In describing his expectation of “how we are going to work with the sector...in every interaction we have”, Dr Bloomfield’s key word is “respectful”.
The leadership is “not about command and control, but convene and collaborate”, he says.
“The ministry has got a critical role in convening people to help achieve outcomes, solve problems and progress the sector. And that, for me, summarises it, and I have been able to make that really clear to staff.”
On health care homes and similar new approaches: It wouldn’t be of any value whatsoever, if it wasn’t changing the way practices feel about their ability to deliver services to their population
LEADING PUBLIC health academic Peter Crampton has (in his own words) “a great interest in and engagement with health policy”. In recent years, Professor Crampton says, he has struggled to engage with the ministry.
He and University of Otago colleagues want to support Dr Bloomfield in his challenging task. Professor Crampton finds him approachable and committed to a highly performing health system, saying he has integrity, deep insight, system and policy knowledge, and management skills.
Similarly impressed, Bridget Allan, chief executive at Hutt Valley’s Te Awakairangi Health Network, is sad to have lost Dr Bloomfield from her local DHB.
“I have always found him extremely constructive and forward-looking, and he has a good understanding of primary care,” Ms Allan says.
That understanding has deepened across DHBs, she says, with Nick Chamberlain (Northland DHB boss and former GP) leading the steering group for DHBs’ national work on primary care; Dr Bloomfield was his deputy.
He was also a DHB member of the PHO Services Agreement Amendment Protocol (PSAAP) group, which negotiates contract changes in primary care and general practice.
In a former life, Cathy O’Malley, a Nelson Marlborough DHB senior manager, moved from Compass Health PHO to the ministry in 2012. Ms O’Malley arrived to find Dr Bloomfield regarded as legendary for his work on tobacco control.
Alongside the fact he has since run a coalface organisation, his experience of the political process is crucial, Ms O’Malley believes, saying many people underestimate the importance of working closely with ministers.
She expects he will make a “fantastic” director-general.
On the latest Health and Independence Report 2017: Our big challenge is around ongoing inequities
DR BLOOMFIELD acknowledges GPs have high expectations of a “fundamental look at the way primary care is funded”.
It’s an ongoing discussion with primary care, he says.
Health minister David Clark has already moved a promised primary care funding review into the broader sector review being led by public service veteran Heather Simpson.
Ms Simpson’s interim report is due in a year’s time, but the final report won’t reach Dr Clark until about January 2020.
The reviewers have been asked to consider the importance of primary healthcare as the foundation of a person-centred health and disability system.
Primary care people expect their part of the sector will be looked at early in the review process, Dr Bloomfield says. Again, “that conversation is ongoing”.
He sees the ministry as playing a key role “facilitating really good primary care input into, and engagement with, that review”.
Dr Bloomfield admits the stated intention of a more prominent role for primary care hasn’t eventuated. The incentives and pressures haven’t allowed it to happen, he says.
“There probably wasn’t the focus on what would be needed in terms of workforce – not just the general practice workforce, but creating a wider range of roles – nursing, pharmacy and allied health – to support that model.
“I think we are in a different place now.”
IN SOME DHBs, strong primary–secondary alliances are encouraging and are paying off, Dr Bloomfield says.
DHBs that have funded health care home-type approaches are “shifting the game”. They’re the way of the future, he says. While not yet fully evaluated, research into health care homes so far has had promising results.
“But most profound for me is the feedback you get from practices who embark on this process. It does, from their perspective, make a difference...
“It wouldn’t be of any value whatsoever, if it wasn’t changing the way they feel about their ability to deliver services to their population.”
Elements such as GP triage, long-term conditions care planning and extended hours, coupled with patient portal use, help primary care to deliver services differently, at quite a modest DHB/ PHO investment, he says.
Dr Bloomfield sees an even bigger opportunity ahead: enabling district nurses and other allied health professionals to be “deployed much more around a primary and community service, rather than accessed through the hospital”.
Beyond this, he would like to see the ministry let go of many of its contracts with local providers, so DHBs and PHOs can do the job in a more locally aligned way.
A “devolution of funding” policy is being considered, although this can’t pre-empt Ms Simpson’s review and would require approval from the Cabinet.
WHAT IS THE RISK that new initiatives will continue to roll out but not make as much, or perhaps any, difference to the outcomes for the treaty partner, Māori? How concerned is Dr Bloomfield at the equity gap for Māori and Pasifika compared with the New Zealand European?
He says he felt fortunate to be able to put his signature to the newly released Health and Independence Report 2017, and that it shows the health of New Zealanders is continuing to improve.
That document shows amenable mortality for Māori and Pasifika, on latest data, is more than twice the rate of other groups.
Of the report, Dr Bloomfield says: “Our big challenge is around ongoing inequities.”
He says a ministry work programme specifically targets equity, “and not just because it’s one of our minister’s high priorities”.
“This is work that we understand is fundamental to us being able to improve the health and the experience of healthcare in New Zealand.
“The way I would describe it is, it is not okay just to achieve something for the whole population. Achievement incudes delivering for Māori and Pasifika and, if you haven’t delivered for those groups, then you haven’t delivered.
“We will be working really closely with the sector with that expectation...where we look to see improvement happening across a range of domains.”
Dr Bloomfield also says he is seeking views from the ministry’s Māori leadership and staff to advise how best to strengthen the organisation’s Māori capacity and capability. “So you can expect to see some action around that.”
Equity of access to healthcare and wellbeing support was one of the challenges emphasised in the performance review that confirmed the sector’s fears back in December 2017. It will be all eyes on Dr Bloomfield.