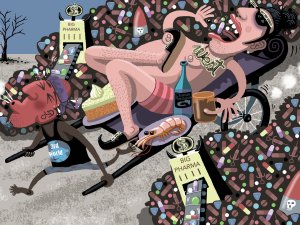
In this article, Sue Frankland looks at the global problem of wastage of medications, including causes such as overprescribing and non-adherence. She also presents information from her master’s dissertation on how people understand, and respond to, medication expiration dates
Study tracks antidepressant use during pregnancy
Study tracks antidepressant use during pregnancy
Almost half of New Zealand women who take antidepressants in the months before getting pregnant, stop during their pregnancy, a new University of Otago study shows.
The research, undertaken by the Pharmacoepidemiology Research Network, published in the Australian and New Zealand Journal of Obstetrics and Gynaecology, used pharmacy dispensing data of more than 800,000 pregnancies to describe patterns of antidepressant use in women before, during and after their pregnancies.
They found that antidepressant use in the nine months prior to pregnancy was stable but dropped considerably during the first trimester and further in the later trimesters. Use then rebounded within the first three months after pregnancy and continued to rise during the first postnatal year.
Lead author Dr Sarah Donald, of the Department of Preventive and Social Medicine, says evidence from a longitudinal study suggests that about 12 per cent of women in New Zealand experience depression, but this study revealed fewer than 5 per cent were using an anti-depressant at any time during pregnancy.
Effective management of depression throughout pregnancy is crucial, she says.
“Although the use of antidepressants in pregnancy does carry a small risk of adverse effects, active depression during pregnancy has also been associated with poorer outcomes; suicide is the leading cause of maternal death in New Zealand, antenatal depression is a risk factor for postnatal depression, and uncontrolled depression during pregnancy also poses risks for infant wellbeing including preterm birth, low birth weight and reduced breastfeeding initiation.
“Our study found that almost half (49 per cent) of women on an antidepressant prior to pregnancy did not continue their antidepressant during pregnancy, but for some of those women, the benefits of continuing may have outweighed the risks,” Dr Donald says.
There was an also an increase in the overall use of antidepressant medication during pregnancy, rising from 3.1% in 2005 to 4.9% by 2014.
“The increasing proportion of women taking an antidepressant during pregnancy is likely a reflection of use in the general population, which has also risen over time. However, we have shown that a lower proportion of pregnant women use an antidepressant compared to the general population.”
The study also revealed there were differences in use by demographic characteristics.
“Younger women and those of Māori, Pacific or Asian ethnicity were less likely to be dispensed an antidepressant before, during, and after pregnancy,” she says.
“Additionally, we found that pregnant women in those groups who were taking an antidepressant before pregnancy were less likely to continue with their antidepressant past early pregnancy.”
One question raised by the study, is what level of antidepressant use in pregnancy is optimal, Dr Donald says.
“We know that having uncontrolled depression during pregnancy carries several risks, so it is important that affected women manage their symptoms. However, for some women, it may be more appropriate to participate in therapy instead of pharmacological treatments if their symptoms are mild.
“We were not able to determine how many pregnant women were accessing non-pharmacological treatments like counselling or therapy, therefore it is difficult for us to assess whether recognition and treatment of depression during pregnancy in New Zealand is adequate from this single study. Future research would be required to explore that issue.”
The study, Antidepressant dispensing before, during and after pregnancy in New Zealand, 2005-2014, was funded by a Clinical Research Training Fellowship from the Health Research Council of New Zealand.