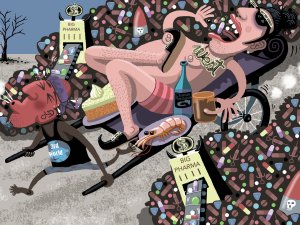
In this article, Sue Frankland looks at the global problem of wastage of medications, including causes such as overprescribing and non-adherence. She also presents information from her master’s dissertation on how people understand, and respond to, medication expiration dates
HPV screening delays mean Māori and Pacific women are dying
HPV screening delays mean Māori and Pacific women are dying
New Zealand’s Māori and Pacific women are dying at two-three times the rate of other women because the way we screen for cervical cancer isn’t as good as it could be.
Dr Samantha Murton is the President of The Royal New Zealand College of General Practitioners and has been ‘frustrated and very disappointed’ by the health system’s lack of progress in this area.
"New Zealand has a world class health system delivering amazing care but, in this respect, we’re letting women, and their families down and that’s particularly true for Māori and Pacific women.
"Cervical screening has progressed and the best first test is now an HPV swab. However, our clinicians are asked to carry on with performing a test that could be done in a better way.
"As a College we expect our members to be working to the best international standards and they currently cannot," says Dr Murton.
Dr Murton, and her colleague Dr Rachel Mackie, who is Chair of Te Akoranga a Māui, the College’s group of Māori doctors, is calling for an urgent Government policy change and investment that would allow women to self-administer a screening test for primary human papillomavirus (HPV). They wish to acknowledge the work of Dr Beverley Lawton (Distinguished Fellow of the College) in her advocacy for implementation of HPV self-testing.
Increased Māori and Pacific deaths have been put down to lower screening rates and studies have shown that a self-taken HPV test is acceptable to Māori women and if provided can increase screening rates by nearly three times.
"The way it works," says Dr Murton, "Is that a woman swabs herself in private, the test gets saved in a plastic tube and handed straight over to the GP or nurse. There has also been research in some places, like Waitematā DHB, about allowing for at-home testing with samples mailed back.
"It’s clean, safe, and private. It is also fantastically cost-effective because you’re not using plastic speculums, disposable bed coverings, or a clinician’s time.
"It’s a real no-brainer," says Dr Murton.
"We can lodge the results the same way a smear test is currently tracked, and we’ll be saving lives."
Dr Rachel Mackie says, "The University of Otago’s Review of Cervical Cancer Occurrences in relation to Screening History in New Zealand for the years 2013-2017 showed a higher incidence of cervical cancer for Māori women compared to non-Māori (8.1 women per 100,000 compared to 4.4 women per 100,000 for non-Māori). This highlights the ongoing equity gap, which continues from previous reviews of cervical cancer rates.
"Mortality rates for Māori are also higher at two-three times that of non-Māori with the numbers being similar for Pacific women. And why? Because of inaction around a simple process change in how women are tested; its inequitable and unacceptable," says Dr Mackie.
"Cervical cancer is an entirely preventable cancer. It is usually a slow-growing cancer so a screening test can pick up changes and allow treatment for precursors prior to the development of cancer but if screening does not occur this cannot happen," she says.
"It doesn’t get much more serious than death and that’s exactly what’s happening to Māori and Pacific women because they’re not being tested enough due to barriers that include this unpleasant examination."
The College wishes to mihi Hon Kiri Allen for being brave enough to share her story so that other women are encouraged to enquire about, or follow up on, cervical screening.
Notes:
- The University of Otago’s Review of Cervical Cancer Occurrences in relation to Screening History in New Zealand for the years 2013-2017 showed a higher incidence of cervical cancer for Māori compared to non-Māori (8.1 women per 100,000) compared to 4.4 women per 100,000 for non-Māori.
- What currently happens: a woman has a smear (cytology) test performed by a nurse or doctor with the results sent to the lab. These are then tested for the precursors to cervical cancer and sometimes HPV but not always.
- What we’re proposing happens: a woman self-administers an HPV test (at her GP’s office or at home) that is then tested at the lab for HPV. Since HPV is the primary indicator of cervical cancer, a cervical smear would only be required if the test was positive or they would be directed straight to colposcopy (a hospital diagnostic test) for some types of HPV depending on the protocol decided by the programme, this direct referral to colposcopy maybe the case for HPV 16 and 18.
- Multiple recommendations from different organisations have been made to start HPV testing:
- The Parliamentary Review Committee Report (April 2019) recommended it to reduce the equity gap
- The Māori Affairs Committee inquiry into health inequities for Māori (2020) recommended it
- Smear your Mea a programme started by Talei Morrison after she was diagnosed with cervical cancer also recommended it.
- The National Cervical Screening Programme was planning to move to primary HPV testing with implementation in 2018 but that has been pushed out to 2021 with no clarity as to when it will happen.