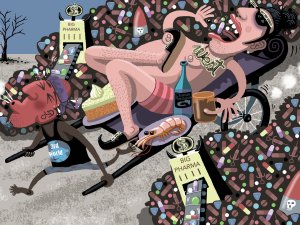
In this article, Sue Frankland looks at the global problem of wastage of medications, including causes such as overprescribing and non-adherence. She also presents information from her master’s dissertation on how people understand, and respond to, medication expiration dates
DHBs to disappear, primary care to get localities – Government announces major health changes
DHBs to disappear, primary care to get localities – Government announces major health changes

DHBs will disappear and primary and community care will be organised in locality networks under New Zealand’s biggest structural health changes in a generation, unveiled by health minister Andrew Little today.
Far from simply reducing the number of DHBs, currently 20, as recommended by last year’s Health and Disability System Review report, the Government will replace them with a new Crown entity, Health New Zealand.
The central body in the health system, Health New Zealand will have four regional divisions, three in the North Island and one in the South. They will commission services from hospitals and Tier 1 (primary and community) services – and fund them. It will also take control of the network of public hospitals.
Alongside Health NZ will be the Māori Health Authority, which, going further than the recommendation of the review, will have the power to commission and fund services.
The Ministry of Health will be slimmed down mainly to a policy and advisory body for the Government, although it will gain a new public health role, being joined up with the 12 public health units at present based in DHBs.
Tier 1 (primary and community) services will be organised in an as-yet-not-defined number of locality networks.
Mr Little says in a media statement, “We are going to put the emphasis squarely on primary and community healthcare and will do away with duplication and unnecessary bureaucracy between regions, so that our health workers can do what they do best – keep people well.
“The reforms will mean that for the first time, we will have a truly national health system, and the kind of treatment people get will no longer be determined by where they live.”
The reforms will be implemented over three years.
Stephen McKernan, the head of the Health and Disability System Transition Unit in the Department of the Prime Minister and Cabinet, tells New Zealand Doctor Rata Aotearoa, responding to a question on who will own locality networks, that this will be determined by the commissioning function of Health NZ in consultation with localities.
A “PHO of the future” could support a locality network, he says, but it would have to be “a bit broader than now”, encompassing aged residential care, pharmacy, home-based support services and other Tier 1 services as identified in the review report.
A government document released today says locality networks will still include GPs, maternity carers, district nurses and optometrists, but the care they provide will be more seamless and accessible.
“That might look like … tightening the connections between care providers, so that records and care pathways follow patients between all those contributing to their care.”
Mr Little says in the release the reforms herald a change in focus. “…we will treat people before they get sick so they don’t need to go to hospital, thereby taking the pressure off hospitals.”
Associate health minister (Māori) Peeni Henare says in the release the Māori Health Authority will have joint decision-making rights to agree on national strategies, policies and plans that affect Maori at all levels of the system and it will work in partnership with Health NZ to ensure that plans and the commissioning of health services drive improvement.
Associate health minister Ayesha Verrall says in the release that the new Public Health Agency will provide technical expertise in the ministry and will act with the public health units as a joined-up national public health service.
Mr Little says, “We know there is more to do – particularly around disability support services and we have asked for more advice on that – and we are committed to working with the sector as we continue to update our health system.”
4 December 2017 – Director-general of health Chai Chuah announces resignation
5 December 2017 – Health minister David Clark appoints a ministerial advisory group on health system
6 December 2017 – Dr Clark says the Performance Improvement Framework Review of the Ministry of Health is an indictment of the previous government’s neglect and under-resourcing
29 May 2018 – Dr Clark announces the Health and Disability System Review, to be led by Heather Simpson
August 2018 – Simpson review panel’s first meeting
27 November 2018 – Ministerial advisory group reports on issues it said should be fixed before completion of the Simpson review
August 2019 – Simpson panel publishes interim report, after holding hearings and receiving written submissions
March 2020 – Final reported completed. The Government, focused on the pandemic, delays receiving it
20 May 2020 – Dr Clark receives the report
16 June 2020 – Dr Clark releases the report, announces formation of Transition Unit to advise on implantation of report’s recommendations
6 September 2020 – Health minister Chris Hipkins announces appointment of former director-general of health Stephen McKernan to lead Transition Unit
21 April 2021 – Health minister Andrew Little announces Government’s health reform plans